The COVID-19 pandemic continues to impact communities across the U.S. and internationally. However, where some countries are trending toward decline in new cases, others—like the U.S—are still reporting new COVID-19 cases.
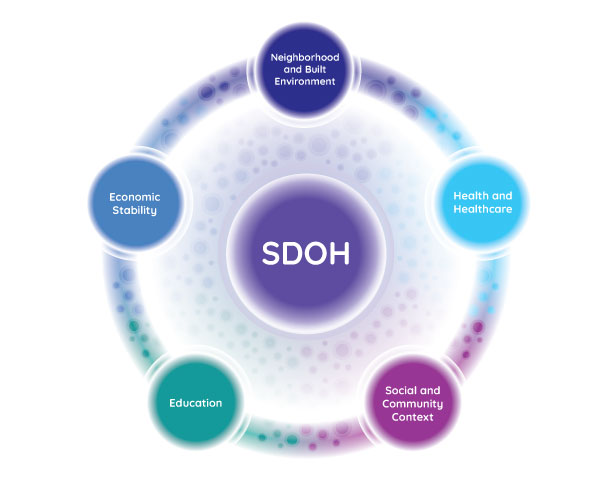
Some areas of the U.S. are affected more than others. This is largely attributed to social determinants of health, which are often out of an individual’s control. Below, we’ve highlighted the five key determinant categories and how each can increase the risk of contracting COVID-19.
The 5 key determinants of health and COVID-19
The following areas represent factors that impact individual and community health. We highlighted a few ways each determinant area could impact communities during the COVID-19 pandemic.
1. Economic stability
Economic stability encompasses employment status, food security, housing stability, and poverty. For most people in the U.S., employment status dictates housing quality, healthcare access, and education opportunities.
But employment does not necessarily guarantee access to stable housing. The average person compensated at minimum wage would have to work nearly 80 hours per week to afford a one-bedroom apartment.
Housing costs cut deeply into many household budgets. For such households, that means less money to spend on healthy food, and potentially more time spent working to cover other expenses. In the COVID-19 pandemic, these budgetary restrictions might mean that households have little money to spend on high-quality or reusable face coverings. It could also mean that some individuals spend more time exposed to the general public through work—increasing their odds of contracting the virus.
2. Education
Education refers to language skills and literacy, high school graduation rates, enrollment in higher education, and access to early childhood development programs.
In March 2020, COVID-19 precautions drove education into the digital realm. Teachers and students became reliant on video calls, email, and other technologies to finish the school year. This sudden disruption was particularly difficult for students in lower-income and rural areas. Students in these areas are less likely to have access to the technologies they need for remote learning.
Experts worry that the shift to digital learning will deepen existing educational disparities. The United Nations estimates that roughly 24 million youth may drop out or otherwise lose access to education solely due to the economic impact of the pandemic.
3. Social and community context
Social and community context includes sociopolitical factors like discrimination, incarceration, civic participation, and social cohesion or solidarity.
Social support and inclusion are vital for mental health and wellbeing. Strict quarantine and social distancing measures began in March 2020 to slow the spread of COVID-19. Research suggests that this social isolation increased symptoms of anxiety, depression, insomnia, post-traumatic stress disorder (PTSD), and other mental health issues.
These negative psychological impacts combined with severe economic impacts are driving cities across the U.S. to reopen businesses—despite reports of new COVID-19 diagnoses.
4. Health and healthcare
Health and healthcare incorporates access to primary and preventative care, access to general healthcare services, and healthcare literacy.
There may be no better time to emphasize the importance of healthcare access than during a pandemic. From a backlog of COVID-19 tests to a scarcity of testing sites in some regions, patients face hurdles even without the complications of insurance coverage.
Fear of contracting the COVID-19 virus is causing many patients to delay essential care. This could mean patients are postponing visits for initial diagnoses or putting off regular appointments. Despite a surge in telemedicine use spurred by the pandemic, patients with restricted access to telehealth technology or who require in-person treatments may face lasting repercussions from postponing care.
5. Neighborhood and built environment
Neighborhood and built environment refers to food access, housing quality, crime and violence rates, and environmental conditions (i.e. air and water quality). Many of the factors in this group are both physical and social determinants.
For several reasons, people living in cities and urban centers may be at higher risk of contracting COVID-19 than those living in rural areas. Because the COVID-19 virus primarily impacts the respiratory system, air pollution could put city dwellers at additional risk. Additionally, crowded living situations, like large apartment buildings with common areas or apartments with many roommates, can increase the risk of exposure.
Housing instability can further increase the risk of COVID-19 exposure. People experiencing homelessness would not have somewhere to safely quarantine or sanitize. Unhoused people may also not have regular access to news alerts and safety recommendations regarding the spread of COVID-19.
How can social determinants of health increase COVID-19 exposure?
Social determinants impact everything from where we grocery shop to the types of employment we pursue. Below, we’ve highlighted specific ways that specific social determinants of health can increase risk of COVID-19 exposure.
1. Public transportation increases COVID-19 exposure
Though many employers turned to remote work to limit the spread of COVID-19, not everyone had this luxury. For essential workers, like healthcare professionals and grocery store employees, working from home is not an option. Of course, there is risk of virus exposure for anyone working with the general public, even with proper use of personal protective equipment (PPE).
The risk of COVID-19 exposure increases for those who rely on public transportation. City buses, cabs, ridesharing services, and other shared modes of transportation often require passengers to sit or stand in close proximity. These vehicles are more difficult to sanitize and may not be cleaned as often as recommended by public health organizations.
Similarly, patients seeking care at nearby hospitals may rely on public transit or ridesharing to attend appointments. These passengers could be at high-risk of developing or suffering complications from COVID-19 and using public transit could increase exposure.
2. Healthcare access decreases likelihood of COVID-19 testing and treatment
As mentioned earlier in this blog, health insurance in the U.S. is largely tied to employment status. For uninsured or underinsured patients, paying for COVID-19 screening tests may be difficult. While some testing sites do accept Medicare and Medicaid, many require appointments and the full testing cost may not be covered.
Additionally, suburban and rural areas may have fewer COVID-19 testing sites than urban areas. This makes it more difficult for patients in these areas to access testing services. Telemedicine use may alleviate this issue. Between June 2019 and June 2020, telemedicine use grew by 2,400 percent.
Top 5 telemedicine procedures in 2020
- CPT code 99442: telephone evaluation by a physician, 11-20 minutes
- CPT code 99441: telephone evaluation by a physician, 5-10 minutes
- CPT code 99443: telephone evaluation by a physician, 21-30 minutes
- CPT code Q3014: telehealth facility fee
- CPT code 93295: interrogation device evaluation, up to 90 days
Fig. 1 Data from Definitive Healthcare’s Medical Claims database. Data is from the calendar year 2020 through June (most recent available). Commercial claims data is sourced from multiple medical claims clearinghouses in the United States. Full list available at Top 25 Telemedicine Procedures During the COVID-19 Pandemic.
3. Poverty limits ability to take time off work and school to avoid COVID-19 exposure
As schools prepare for students to return, many working parents will have to make difficult decisions about whether to keep their children home. Most parents cannot afford to take time off work to homeschool, and many will have to juggle schedules for multiple children. Parents back at work and students back in schools significantly increases the likelihood of COVID-19 exposure.
With some schools moving to a blended syllabus of online and in-person classes, families may struggle to provide access to computers and tablets for multiple children. In addition, more than 22 million U.S. children rely on free or reduced-cost lunches during the school year and may struggle with adequate nutrition if they’re out of school for extended periods—putting them at greater risk of developing long-term health conditions.
Learn more
Are you looking for more information about the impacts of COVID-19 on healthcare delivery and technology? Watch our on-demand webinar, Examining The COVID-Driven Rise of Telehealth With Claims at any time.
Webinar hosts explore:
- What patterns in claims data reveal about the digital expansion of healthcare
- What these observations mean for sales organizations for companies that serve providers
- What current regulations mean for the continued growth in digital utilization





